La medicina generale è ormai sempre piú orientata alla gestione del paziente cronico. A questo proposito una non irrilevante porzione di pazienti con malattie croniche è rappresentata da quelli con scompenso cardiaco. La gran parte dei pazienti con scompenso cardiaco acuto infatti ha una esacerbazione di uno scompenso cronico, con solo il 15-20% di patologie ’’de novo’’. Approssimativamente il 50% dei pazienti con scompenso cardiaco acuto ha una frazione di eiezione conservata. Meno del 5% dei pazienti presentano ipotensione e richiedono terapia con inotropi. Con un tale background, qual è il ruolo del medico di medicina generale in questo setting?
L’intenzione di questo articolo è quindi quella di analizzare la patologia da un punto di vista pratico con accenni diagnostici ma soprattutto terapeutici, tralasciando momentaneamente anamnesi, segni, sintomi, classificazioni e stadiazione (che è possibile trovare al seguente LINK).
LEGENDA: Durante il corso dell’articolo troverete vari avvisi colorati come ”Attenzione” o ”NB”; questi rappresentano suggerimenti pratici o spunti interpretativi da integrare con le varie indicazioni delle linee guida sopra riportate.
Ho un sospetto di Scompenso Cardiaco, quali esami sono necessari per un inquadramento di base (completo)?
L´American College of Cardiology Foundation/American Heart Association (ACFF/AHA) e l´ Heart Failure Society of America (HFSA) assieme all´ European Society of Cardiology (ESC) raccomandano i seguenti test di laboratorio ed approfondimenti al fine dell´inquadramento del paziente con sospetto scompenso cardiaco:
NB: Si riportano gli esami con un breve razionale del perché richiederli a lato
Esami di Laboratorio
-Emocromo (anemia/infezione come cause dello scompenso?)
-Analisi delle urine (proteinuria? Talvolta associata a patologie cardiovascolari)
–Elettroliti (ritenzione di fluidi? Disfunzioni renali?)
–BUN + creatininemia (riduzione dell´afflusso renale?)
–Glicemia a digiuno ( alti livelli possono indicare un aumentato rischio di scompenso cardiaco, sia nei diabetici che nei non diabetici)
–Funzionalitá epatica (disfunzione epatica/congestione da scompenso cardiaco?)
–BNP e NT-proBNP (aumentati nello scompenso cardiaco, stretta correlazione con classificazione NYHA) –>molto utili in caso di dubbio diagnostico in quanto bassi valori rendono improbabile la presenza di scompenso.
–TSH + profilo lipidico
Attenzione: BNP e NT-proBNP hanno probabilmente maggiore valore in una popolazione non selezionata come puó essere quella di un medico di medicina generale piuttosto che in una popolazione di soggetti ad alta probabilità di scompenso come in un reparto di cardiologia dove la loro utilità nel discriminare un reale scompenso cardiaco (o riacutizzazione) rispetto ad altre problematiche è probabilmente molto ridotta (raramente si avranno pazienti con BNP in range).
NB: Se esiste il sospetto di una sindrome coronarica acuta, come raccomandato dalla ESC, é opportuno provvedere ad ottenere livelli di Troponina come indici di danno miocitico.
Attenzione: va tenuto ben presente che la Troponina misurata in una popolazione di scompensati, probabilmente sarà positiva in una buona percentuale (generalmente con valori non elevatissimi, ma comunque decisamente superiori al cut off tradizionale). Quindi occorre che la richiesta di Troponina vada fortemente motivata sulla base del sospetto clinico per non catalogare erroneamente i pazienti come sindromi coronariche acute.
Esami strumentali
-ECG 12 derivazione (aritmia,ischemia/infarto, coronaropatie?)
–Rx del torace (2p PA+LL) (congestione polmonare,immagine cardiaca allargata?)
–Ecocardiografia + doppler (disfunzioni ventricolari/anormalitá valvolari?)
–Arteriografia coronarica in caso di storia di angina o sospetta disfunzione ventricolare sx ischemica (piú frequentemente richiesta giá in ambitio specialistico)
La ESC non suggerisce di eseguire test per la funzione polmonare poiché poco utili nella diagnosi di scompenso cardiaco. Tuttavia questo tipo di esami sono comunque da tenere presente nel caso sia necessario escludere cause polmonari di dispnea.
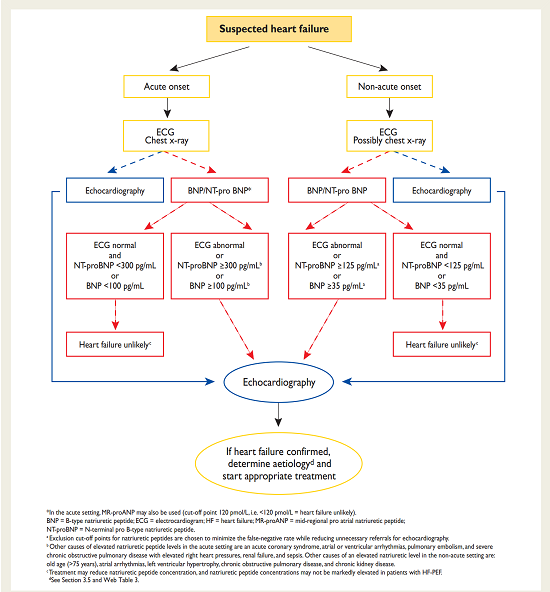
Di seguito si riporta per completezza una breve Flow-chart (linee guida ESC) per una migliore integrazione ed interpretazione degli esami sopra suggeriti
TRATTAMENTO
Scompenso cardiaco acuto
La terapia medica per lo scompenso cardiaco si focalizza nella gran parte dei casi su:
1)riduzione del precarico e del postcarico tramite vasodilatatori e diuretici (con risoluzione a breve termine della sintomatologia)
2)inibizione della cascata neuro-ormonale deleteria quale è quella di renina-angiotensina-adlosterone e quella del sistema simpatico (di Ace inibitori, Betabloccanti e Antagonisti dell´aldosterone).
In caso di scompenso cardiaco acuto la triade terapeutica di base è Ossigeno-Diuretici-Vasodilatatori
NB: Generalmente l´ossigeno é necessario soprattutto in presenza di SaO2 inferiore al 90%
Diuretici
Rappresentano ancora oggi il punto chiave della terapia dello scompenso cardiaco acuto nonché i farmaci di prima linea, il cui capostipite é rappresentato da diuretici dell´ansa (Furosemide, Torasemide ecc ecc).
In questi pazienti NON è consigliata la somministrazione del farmaco per OS poiché il probabile edema dell´intestino potrebbe ostacolarne l´assorbimento con formulazione orale. Le altre forme sono accettate, in particolar modo é suggerita quella endovenosa, la quale rappresenta il gold standard.
NB in pazienti con scompenso cardiaco ipertensivo è possibile utilizzare i diuretici tiazidici (es. metolazone, idroclorotiazide) per il loro maggior effetto antipertensivo nel tempo.
La dose (20-200 mg/die) e la frequenza dei diuretici è molto variabile e dipende dalla risposta del paziente dopo 2-4 h, non é saggio quindi fornire uno standard universale. Se la diuresi permane inadeguata si raccomanda un aumento di dose o l´aggiunta di un diuretico tiazidico, anche se in generale è sempre meglio evitare l’associazione tra diuretici dell’ansa e tiazidici, a meno che sia possibile controllare frequentemente elettroliti e creatinina, poiché il rischio di ipopotassiemie è tangibile.
NB: l´equivalenza tra Furosemide e Torasemide è circa di 2:1 , ovvero 40 mg/die di Furosemide equivalgono a circa 20 mg di Torasemide. L´equivalenza tra Furosemide endovena/i.m e Furosemide per OS è di 1:2, ovvero 20 mg e.v. equivalgono a 40 per OS, mentre la Torasemide ha equivalenza Os:e.v/ di 1:1.
Attenzione: Se il paziente con scompenso è iperteso non è per forza un male!!! Significa maggior spazio per la titolazione della ”vera terapia antiscompenso’’ (es. ACE-inibitori, Betabloccanti ecc.), la quale è l´unica in grado di modificare la storia della malattia.
Vasodilatatori
Raccomandati come adiuvanti alla terapia diuretica con la seguente restrizione:
Cautela al loro uso nei pazienti con Pressione Sistolica < a 100 mmHg o con significativa stenosi mitralica o aortica
1)I nitrati sono potenti venodilatatori e vasodilatatori coronarici. Possono essere usati in diverse forme (sublinguale, orale, transdermica ecce cc) ma in questa condizione la via suggerita rimane comunque, ove possibile, l´endovenosa.
2)Il Nitroprussiato sodico è un potente farmaco dilatatore arterioso, particolarmente utile per i pazienti che presentano congestione polmonare severa, ipertensione e rigurgito mitralico. Purtroppo necessita di un attento monitoraggio sia emodinamico che per la tossicitá (cianidi).
Attenzione: Nello scompenso acuto, al di là di ciò che dicono le linee guida, non è così frequente avere lo spazio all’utilizzo reale dei vasodilatatori e.v. Questo perché i pazienti sono generalmente ipotesi e non conviene ”giocarsi nell’uso del nitrato’’ quei pochi mmHg di PA che invece possono servire alla titolazione della terapia antiscompenso senza rischiare di creare ipotensione sintomatica ( es. ipoperfusione renale). Al contrario, è molto più frequente l’utilizzo degli inotropi, tipici del setting ospedaliero. Diverso invece il caso di paziente iperteso, nel qual caso i nitrati possono avere un maggiore spazio.
Ma posso davvero trattare fuori dall´ospedale uno scompenso cardiaco acuto?
In linea generale un paziente che risulta refrattario alla terapia standard necessita sempre di ospedalizzazione al fine di ricevere diuretici, vasodilatatori e agenti inotropi e.v. in un regime controllato.
L´ Heart Failure Society of America (HFSA) raccomanda l´ospedalizzazione per lo scompenso cardiaco acuto in caso di:
-Scompenso acuto severo (bassa pressione, riduzione funzionalitá renale,alterazione attivitá mentale)
-Dispnea a riposo
-Aritmie emodinamicamente significative-Sindrome coronarica acuta
-Congestione in peggioramento con o senza dispnea-Peggioramento dei segni e sintomi della congestione sistemica o polmonare, anche in assenza di aumento di peso
-Anormalitá maggiori degli elettroliti-Presenza di comorbiditá (es. Polmonite,embolia polmonare, chetoacidosi diabetica, stroke, sintomi stroke-like)
-Nuova diagnosi di scompenso cardiaco CON segni di congestione attività sistemica/polmonare
-Ripetute scariche dell´ ICD (implantable-cardioverter-defibrillator)
Da questo se ne deduce come i casi di scompenso acuto che possono essere gestiti sul territorio sono molto limitati (se non virtuali), tuttavia un precoce e corretto inquadramento grazie alle indagini di base indicate in precedenza potrebbe accelerare il processo diagnostico portando ad un intervento terapeutico piú rapido in massima sinergia con gli specialisti e le strutture ospedaliere.
Scompenso cardiaco cronico Sx con ridotta Frazione di Eiezione
TRATTAMENTO FARMACOLOGICO
Il trattamento farmacologico di pressoché ogni tipo di scompenso cardiaco è il seguente e puó essere riassunto in TRE regole fondamentali:
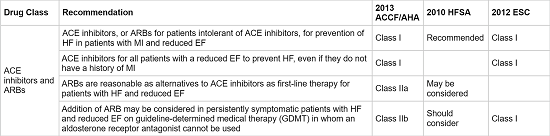
UNO: In tutti i pazienti con FE (frazione di eiezione) < 40% l´uso di un Ace inibitore o Sartanico (ARBs) in aggiunta ad un betabloccante é consigliato.
DUE: Un Antagonista del recettore dei mineralcorticoidi dovrebbe essere utilizzato in tutti i pazienti con sintomi persistenti (NYHA II-IV) nonostante l’utilizzo di Ace inibitori e Betabloccante. In caso di impossibilitá all’utilizzo di un Antagonista dei mineralcorticoidi é possibile tentare l’aggiunta di un Sartanico (doppio blocco Ace-inibitori + Sartanico)
TRE: Se vi é persistenza di sintomi o intolleranza a Betabloccanti + Frequenza Cardiaca > 75 bpm (ritmo sinusale) + FE molto depressa (< 35%) é suggerito l’uso di Ivabradina
Attenzione: Nella visione attuale, per parlare di scompenso cardiaco a FE preservata (HFpEF), la FE deve essere davvero preservata (cioè >50%) in tutti gli altri casi in cui c’è disfunzione sistolica si parla comunqe di HF classico (HFrEF). Il cut off del 40% era ed è ancora riportato in alcune linee guida perché nei vecchi studi sullo scompenso sistolico venivano tendenzialmente arruolati solo pazienti con FE severamente compromessa, mentre nella visione attuale tale limite è stato progressivamente innalzato (fino ad arrivare all’attuale concetto della “reale” preservazione della FE).In realtà, per quegli stessi motivi (e in una visione più concreta e attuale) i benefici di questi farmaci probabilmente si estendono a tutti i pazienti con Scompenso Cardiaco e FE ridotta (ovvero <50%);
NB: La digitale può essere data nei casi di Scompenso Cardiaco a Frazione di Eiezione preservata in caso di persistenza dei sintomi nonostante terapia ottimale. In realtà,visto il trade-off tra rischio/beneficio si tende ad usare solo nei pazienti con HFpEF + fibrillazione atriale (generalmente in una strategia di controllo della FC).
ACE INIBITORI/ARBs
Si riportano le dosi Target di alcune molecole che hanno dimostrato di aumentare la sopravvivenza/ridurre la mortalitá/ridurre ospedalizzazioni.Importante è iniziare da una dose più bassa (di partenza) andando a crescere nel tentativo del raggiungimento della dose target (titolazione).
Ace inibitori
Captopril: 25/50 mg TID (dose di partenza 6,25 mg TID)
Enalapril 10/20 mg BID (dose di partenza 2,5 mg BID)
Lisinopril 20/35 mg/die (dose di partenza 2,5/5 mg/die)
Ramipril 5 mg BID (dose di partenza 2,5 mg/die)
NB: Le maggiori evidenze sono comunque a carico degli Ace inibitori che sono quindi sempre da preferire
ARBs
Valsartan 160 mg BID (dose di partenza 40 mg/die)
Candesartan 32 mg/die (dose di partenza 4/8 mg/die)
Attenzione: Dopo l’avvio di Ace inibitori (o Sartanici), un certo grado di peggioramento della creatinina rispetto al basale, nei limiti di normalitá, può essere atteso, e non deve indurre alla sospensione (o alla riduzione) del farmaco, a patto che tale peggioramento si stabilizzi su valori accettabili.
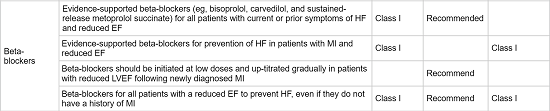
BETA BLOCCANTI
Si riportano le dosi Target di alcune molecole che hanno dimostrato di aumentare la sopravvivenza/ridurre la mortalitá/ridurre ospedalizzazioni. Importante è iniziare da una dose più bassa (di partenza) andando a crescere nel tentativo del raggiungimento della dose target (titolazione).
Con azione alfa 1 bloccanti:
Carvedilolo 25-50 mg BID (dose di partenza 3,125 mg BID)
Selettivi per recettori Beta-1:
Metoprololo 200 mg/die (rilascio prolungato) (dose di partenza 12,5/25 mg/die)
Bisoprololo 10 mg/die (dose di partenza 1,25 mg/die)
Attenzione: In generale, tra i betabloccanti, nello scompenso il più usato è il Bisoprololo. Al contrario il Carvedilolo determina maggior ipotensione (e quindi meno possibilità di titolazione), per quanto riguarda il Metoprololo si tende a preferire di solito nei pazienti con cardiopatia ischemica.
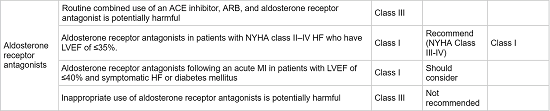
ANTAGONISTI ALDOSTERONE
Si riportano le dosi Target di alcune molecole che hanno dimostrato di aumentare la sopravvivenza/ridurre la mortalitá/ridurre ospedalizzazioni. Importante è iniziare da una dose più bassa (di partenza) andando a crescere nel tentativo del raggiungimento della dose target (titolazione).
Eplerenone 50 mg/die (dose iniziale 25 mg/die)
Attenzione: A dispetto di ciò che dicono le linee guida, in Italia si usa sostanzialmente lo Spironolattone (spesso in associazione con la Furosemide, dose standard 25+37 mg/die), oppure, il Canrenone (metabolita dello Spironolattone) 50/100 mg/die, il quale tuttavia non ha alla base citazioni in grandi studi.
IVABRADINA
Dose iniziale 5 mg BID valutando Frequnza Cardiaca dopo circa 2 settimane:
– FC tra 50-60 bpm: mantengo la dose
– FC < 50 bpm: riduco la dose a 2,5 mg BID
– se > a 60 bpm: aumento la dose a 7,5 BID
Attenzione: Per una questione di sicurezza il Target di Frequenza Cardiaca é verosimilmente meglio tenerlo ai limiti superiori intorno ai 60 bpm (senza superare i 70 bpm) in modo da non ridurre troppo la portata cardiaca, dato che il paziente non puó essere monitarato h 24 e le variazioni di frequenza circardiane sono molteplici.
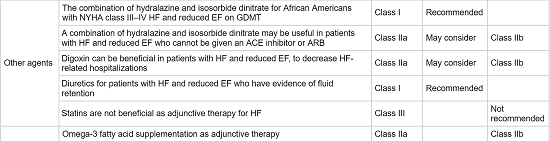
ALTRI
Dosi piú comunemente utilizzate, tenendo ben presente che in questo caso il target è mantenere l´euvolemia del paziente o il cosiddeto ‘’dry weight’’ con la minor dose possibile di diuretico, evitando disidratazione, ipotensione e disfunzione renale.
Diuretici dell´ansa:
Furosemide 40-240 mg (dose di partenza 20-40 mg/die)
Torasemide 10-20 mg (dose di partenza 5-10 mg/die)
Diuretici Tiazidici:
Idroclorotiazide 12,5-100 mg (dose di partenza 25 mg/die)
Indapamide 2,5-5 mg (dose di partenza 2,5 mg/die)
NB: se un diuretico potassio disperdente è utilizzato in concomitanza a Ace inibitori (o Sartanici) e Antagonisti dell´Aldosterone la supplementazione di potassio sovente non è necessaria. Non è consigliato invece generalmente utilizzare diuretici risparmiatori di potassio assieme a Ace inbitori (o Sartanici) e Antagonisti dell´Aldosterone.
Attenzione: Importantissimo é il costante e preciso monitoraggio della dose dei diuretici anche mediante l´automisurazione del peso del paziente (cosa in cui alcuni pazienti possono essere educati). In caso di ipotensione sintomatica é corretto ridurre la dose del diuretico piuttosto che sospendere i veri farmaci ”antiscompenso” quale per esempio Ace inibitori e Betabloccanti, ma sempre con prudenza e attenzione perché la riduzione troppo brusca o eccessiva determina riacutizzazione dello scompenso stesso.
NB: in questo articolo non si parlerá di TAO; in linea molto generale la sola depressione della Frazione di Eiezione in assenza di fattori di rischio/indicazioni a scoagulazione non sono fattori sufficienti a giustificarne l’inizio.
Farmaci non raccomandati
L´ ACCF/AHA e l´ESC sconsigliano fortemente l´uso di:
1)FANS (attenzione anche ai prodotti da banco, che i pz tendono ad assumere al bisogno talvolta con leggerezza)
2)Antiaritmici (tra questi ultimi l´Amiodarone ha dimostrato uni dei profili piú sicuri)
3)Calcioantagonisti (I Diidropiridinici tuttavia, come Amlodipina e la Barnidipina, possono essere considerati relativamente sicuri per il trattamento dell´ipertensione o delle patologie ischemiche in questi pazienti)
4)Tiazolidinedioni: non dovrebbero essere impiegati per trattare pazienti con diabete mellito e scompenso cardiaco.
NB: Particolare attenzione anche alle terapia con Corticosteroidi in particolar modo se a dosi elevate e per periodo prolungato. Antidolorifici suggeriti: Paracetamolo, Oppiodi, cardioASA.
Attenzione: Prima di procedere occorre sottolineare che le dosi consigliate come ”target” nelle linee guida sono difficilmente raggiungibili nella ”vita reale”,poiché i pazienti inclusi nei trial sono spesso purtroppo profondamente diversi dai pazienti reali. La titolazione del farmaco va tuttavia tentata ed eventualmente mantenuta ad un dosaggio inferiore, che rappresenti peró il miglior livello di sicurezza per il paziente. Il Medico di Medicina Generale ha un ruolo fondamentale in questa fase della cura del paziente. Infatti spesso i pazienti vengono dimessi dagli ospedali ancora in fase di titolazione (con ampi margini per ottimizzarla); la terapia non si dovrebbe quindi cristallizzare su quella delineata nella lettera di dimissione
TRATTAMENTO NON FARMACOLOGICO
1)Trattare ipertensione e disordini lipidici
2)Incoraggiare la cessazione del fumo
3)Scoraggiare l´uso di alcol e droghe
4)Promuovere controllo e prevenzione ottimali di diabete mellito, insulino-resistenza e rischio vascolare
5)Incoraggiare attivitá fisica aerobica al fine di migliorare le capacitá funzionale e i sintomi. L’attività fisica tuttavia dovrebbe essere limitata durante l’esacerbazione di scompenso cardiaco e in pazienti con sospetta miocardite
6)Incoraggiare la perdita di peso se il paziente è obeso o sovrappeso
7)Il sodio nella dieta dovrebbe essere ridotto a 2-3 g/die in accordo con ACCF/AHA,ESC e HFSA
8)La quota totale di fluidi non dovrebbe superare i 2 L/die per i pazienti con evidenza di iponatremia (<130 mEq/dL) e per i soggetti il cui ”fluid status’’ è difficile da controllare nonostante la restrizione di sodio e l´uso di alte dosi di diuretici.
Scompenso cardiaco cronico sx con Frazione di Eiezione conservata
Attualmente quasi nessun trattamento ha dimostrato in modo convincente di ridurre morbiditá e mortalitá in pazienti con Scompenso Cardiaco e FE conservata. Il trattamento è infatti fondamentalmente indirizzato ad alleviare i sintomi.
1)La terapia diuretica rimane comunque raccomandata per ridurre la ritenzione di fluidi.
2)Ace inibitori/Sartanici sono generalmente i piú indicati per i pazienti diabetici, ipertesi, con pregresso infarto miocardico, o con aterosclerosi. Candesartan, Irbesartan o Perindopril non hanno dimostrato di ridurre la mortalitá ma hanno prodotto un primo trend di miglioramento per quanto riguarda la morbiditá e le ospedalizzazioni. Alcune evidenze mostrano come Losartan e Valsartan potrebbero promuovere un miglioramento nella funzione diastolica riducendo l´ipertrofia ventricolare sinistra.
3)I Betabloccanti sono indicati per i pazienti con pregresso infarto miocardico o ipertensione e per il controllo della frequenza.
4)I Calcioantagonisti non sembrerebbero controindicati.
NB nel registro ADHERE i soggetti trattati con Betabloccanti hanno dimostrato una piú alta mortalitá. Le modifiche dello stile di vita (vedi “Trattamento non farmacologico”) suggerite per lo scompenso cardiaco a frazione di eiezione ridotta valgono in linea di massima anche per lo scompenso a frazione di eiezione conservata.
Quali accorgimenti avere invece in un paziente con decompensazione di uno scompenso giá noto (ADHF)?
L´ACCF/AHA raccomanda quanto segue:
1)La terapia orale dovrebbe essere continuata ed eventualmente aumentata nella gran parte dei pazienti con scompenso cardiaco con ridotta frazione di eiezione.
2)Continuare Ace inibitori o Sartanici e betabloccanti poiché statisticamente ben tollerati e associati ad outcomes migliori nella gran parte dei pazienti
3)Sospensione di beta-bloccanti o riduzione di dose dovrebbe essere considerata SOLO in pazienti ospedalizzati dopo un recente inizio di beta-bloccanti o un recente aumento di dosaggio, oppure nei soggetti con franco sovraccarico di volume o basso output cardiaco
4)Nei pazienti con significativa riduzione della funzionalitá renale, la riduzione di dose temporanea o interruzione di Ace inibitori, Sartanici e/o Antagonisti dell´Aldosterone dovrebbe essere considerata fino al miglioramento della funzione renale
AUTORE
Daniele Angioni
Si ringrazia la dott.ssa Silvia Busceti per l’aiuto fornito alla realizzazione di questo articolo
Un ringraziamente speciale al Dott. Enrico Boggio (spec.ndo Cardiologia) che ha contribuito alla revisione di questo articolo in nome della sinergia tra specialisti e medici di medicina generale, preziosi alleati per la gestione e la cura ottimale del paziente.
BIBLIOGRAFIA
Medscape Heart Failure Guidelines Henry H Ooi, MDFramingham Classification: Ho KK, Pinsky JL, Kannel WB, Levy D. The epidemiology of heart failure: the Framingham Study. J Am Coll Cardiol. 1993 Oct. 22(4 Suppl A):6A-13A. [Medline].American Heart Association. Classes of heart failure. Available athttp://www.heart.org/HEARTORG/Conditions/HeartFailure/AboutHeartFailure/Classes-of-Heart-Failure_UCM_306328_Article.jsp. Accessed: September 6, 2011.[Guideline] Hunt SA, Abraham WT, Chin MH, et al, and the American College of Cardiology Foundation; American Heart Association. 2009 Focused update incorporated into the ACC/AHA 2005 guidelines for the diagnosis and management of heart failure in adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines developed in collaboration with the International Society for Heart and Lung Transplantation. J Am Coll Cardiol. 2009 Apr 14. 53(15):e1-e90. [Medline].[Guideline] Hunt SA, for the Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure). ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2005 Sep 20. 46(6):e1-82. [Medline].[Guideline] Dickstein K, Cohen-Solal A, Filippatos G, et al. for the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur Heart J. 2008 Oct. 29(19):2388-442. [Medline].[Guideline] Lindenfeld J, Albert NM, Boehmer JP, et al, for the Heart Failure Society of America. Executive summary: HFSA 2010 comprehensive heart failure practice guideline. J Card Fail. 2010 Jun. 16(6):e1-194.[Medline].Stiles S. FDA Approves Heart Sympathetic Activity Imaging Agent for HF Evaluation. Available athttp://www.medscape.com/viewarticle/781309. Accessed: April 5, 2013.Braunwald E. The pathogenesis of heart failure: Then and now. Medicine. 1991. 70:68.Braunwald E, Ross J Jr, Sonnenblick EH. 2 ed. Mechanisms of Contraction of the Normal and Failing Heart. Boston: Little Brown & Co; 1976. 417.Clifford R Greyson, MD. Pathophysiology of right ventricular failure. Crit Care Med. 2008. 36(suppl):S57-65.Haddad F, Doyle R, Murphy DJ, Hunt SA. Right ventricular function in cardiovascular disease, part II: pathophysiology, clinical importance, and management of right ventricular failure. Circulation. 2008 Apr 1. 117(13):1717-31. [Medline].Onwuanyi A, Taylor M. Acute decompensated heart failure: pathophysiology and treatment. Am J Cardiol. 2007 Mar 26. 99(6B):25D-30D. [Medline].Ross J Jr, Braunwald E. Studies on Starling’s law of the heart. The effects of impeding venous return on performance of the normal and failing human left ventricle. Circulation. 1954. 30:719.Gheorghiade M, Pang PS. Acute heart failure syndromes. J Am Coll Cardiol. 2009 Feb 17. 53(7):557-73.[Medline].Kajstura J, Leri A, Finato N, Di Loreto C, Beltrami CA, Anversa P. Myocyte proliferation in end-stage cardiac failure in humans. Proc Natl Acad Sci U S A. 1998 Jul 21. 95(15):8801-5. [Medline]. [Full Text].Cohn JN. Structural basis for heart failure. Ventricular remodeling and its pharmacological inhibition.Circulation. 1995 May 15. 91(10):2504-7. [Medline].Cody RJ. Hormonal alterations in heart failure. Hosenpud JB, Greenberg BH, eds. Congestive Heart Failure: Pathophysiology, Diagnosis and Comprehensive Approach to Management. Philadelphia: Lippincott Williams & Wilkins; 2000. 199-212.Anversa P, Nadal-Ginard B. Myocyte renewal and ventricular remodelling. Nature. 2002 Jan 10. 415(6868):240-3. [Medline].Leri A, Claudio PP, Li Q, Wang X, Reiss K, Wang S, et al. Stretch-mediated release of angiotensin II induces myocyte apoptosis by activating p53 that enhances the local renin-angiotensin system and decreases the Bcl-2-to-Bax protein ratio in the cell. J Clin Invest. 1998 Apr 1. 101(7):1326-42. [Medline].[Full Text].Kajstura J, Leri A, Castaldo C, Nadal-Ginard B, Anversa P. Myocyte growth in the failing heart. Surg Clin North Am. 2004 Feb. 84(1):161-77. [Medline].Henes J, Rosenberger P. Systolic heart failure: diagnosis and therapy. Curr Opin Anaesthesiol. 2016 Feb. 29 (1):55-60. [Medline].Nicoara A, Jones-Haywood M. Diastolic heart failure: diagnosis and therapy. Curr Opin Anaesthesiol. 2016 Feb. 29 (1):61-7. [Medline].Feldman AM, Combes A, Wagner D, Kadakomi T, Kubota T, Li YY, et al. The role of tumor necrosis factor in the pathophysiology of heart failure. J Am Coll Cardiol. 2000 Mar 1. 35(3):537-44. [Medline].Rebecca Gary, RN, PhD, Leslie Davis, MSN, RN, et al. Diastolic heart failure. Heart & Lung. 2007. 37(6):405-16.Morris DA, Gailani M, Vaz Perez A, et al. Right ventricular myocardial systolic and diastolic dysfunction in heart failure with normal left ventricular ejection fraction. J Am Soc Echocardiogr. 2011 Aug. 24(8):886-97.[Medline].Lam CS, Lyass A, Kraigher-Krainer E, et al. Cardiac dysfunction and noncardiac dysfunction as precursors of heart failure with reduced and preserved ejection fraction in the community. Circulation. 2011 Jul 5. 124(1):24-30. [Medline].Ho KK, Anderson KM, Kannel WB, Grossman W, Levy D. Survival after the onset of congestive heart failure in Framingham Heart Study subjects. Circulation. 1993 Jul. 88(1):107-15. [Medline].Halley CM, Houghtaling PL, Khalil MK, Thomas JD, Jaber WA. Mortality rate in patients with diastolic dysfunction and normal systolic function. Arch Intern Med. 2011 Jun 27. 171(12):1082-7. [Medline].Murphy RT, Starling RC. Genetics and cardiomyopathy: where are we now?. Cleve Clin J Med. 2005 Jun. 72(6):465-6, 469-70, 472-3 passim. [Medline].Roger VL, Go AS, Lloyd-Jones DM, et al, for the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2011 update: a report from the American Heart Association. Circulation. 2011 Feb 1. 123(4):e18-e209. [Medline].Fonarow GC. Epidemiology and risk stratification in acute heart failure. Am Heart J. 2008 Feb. 155(2):200-7. [Medline].Gottlieb SS, Khatta M, Friedmann E, Einbinder L, Katzen S, Baker B, et al. The influence of age, gender, and race on the prevalence of depression in heart failure patients. J Am Coll Cardiol. 2004 May 5. 43(9):1542-9. [Medline].He J, Ogden LG, Bazzano LA, Vupputuri S, Loria C, Whelton PK. Risk factors for congestive heart failure in US men and women: NHANES I epidemiologic follow-up study. Arch Intern Med. 2001 Apr 9. 161(7):996-1002. [Medline].Masoudi FA, Havranek EP, Smith G, Fish RH, Steiner JF, Ordin DL, et al. Gender, age, and heart failure with preserved left ventricular systolic function. J Am Coll Cardiol. 2003 Jan 15. 41(2):217-23. [Medline].Ni H, Xu J. Recent trends in heart failure-related mortality: United States, 2000–2014. Centers for Disease Control and Prevention. Available at http://www.cdc.gov/nchs/data/databriefs/db231.htm. December 31, 2015; Accessed: January 5, 2016.Brauser D. CDC: Heart-failure–related mortality rate climbs after decade-long decrease. Heartwire from Medscape. Available at http://www.medscape.com/viewarticle/856704. January 4, 2016; Accessed: January 5, 2016.Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998-2008. JAMA. 2011 Oct 19. 306(15):1669-78. [Medline].Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009 Apr 2. 360(14):1418-28. [Medline].Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, et al. Executive summary: heart disease and stroke statistics–2010 update: a report from the American Heart Association. Circulation. 2010 Feb 23. 121(7):948-54. [Medline].Stewart S, Wilkinson D, Hansen C, Vaghela V, Mvungi R, McMurray J, et al. Predominance of heart failure in the Heart of Soweto Study cohort: emerging challenges for urban African communities. Circulation. 2008 Dec 2. 118(23):2360-7. [Medline].Damasceno A, Cotter G, Dzudie A, Sliwa K, Mayosi BM. Heart failure in sub-saharan Africa: time for action.J Am Coll Cardiol. 2007 Oct 23. 50(17):1688-93. [Medline].Cardiovascular Diseases. Dean T. Jamison, Richard G. Feachem, Eduard R. Bos, Malegapuru W. Makgoba, Florence K. Baingana, Karen J. Hofman, Kahma O. Rogo. Disease and mortality in Sub-Saharan Africa. Washington D.C: World Bank Publications; 2006. 2: 21.Dries DL, Exner DV, Domanski MJ, Greenberg B, Stevenson LW. The prognostic implications of renal insufficiency in asymptomatic and symptomatic patients with left ventricular systolic dysfunction. J Am Coll Cardiol. 2000 Mar 1. 35(3):681-9. [Medline].Fonarow GC, Adams KF Jr, Abraham WT, Yancy CW, Boscardin WJ. Risk stratification for in-hospital mortality in acutely decompensated heart failure: classification and regression tree analysis. JAMA. 2005 Feb 2. 293(5):572-80. [Medline].Levy D, Kenchaiah S, Larson MG, Benjamin EJ, Kupka MJ, Ho KK, et al. Long-term trends in the incidence of and survival with heart failure. N Engl J Med. 2002 Oct 31. 347(18):1397-402. [Medline].Lucas C, Johnson W, Hamilton MA, Fonarow GC, Woo MA, Flavell CM, et al. Freedom from congestion predicts good survival despite previous class IV symptoms of heart failure. Am Heart J. 2000 Dec. 140(6):840-7. [Medline].MacIntyre K, Capewell S, Stewart S, Chalmers JW, Boyd J, Finlayson A, et al. Evidence of improving prognosis in heart failure: trends in case fatality in 66 547 patients hospitalized between 1986 and 1995.Circulation. 2000 Sep 5. 102(10):1126-31. [Medline].Ketchum ES, Levy WC. Establishing prognosis in heart failure: a multimarker approach. Prog Cardiovasc Dis. 2011 Sep-Oct. 54(2):86-96. [Medline].van Diepen S, Bakal JA, McAlister FA, Ezekowitz JA. Mortality and readmission of patients with heart failure, atrial fibrillation, or coronary artery disease undergoing noncardiac surgery: an analysis of 38 047 patients. Circulation. 2011 Jul 19. 124(3):289-96. [Medline].Bursi F, McNallan SM, Redfield MM, et al. Pulmonary pressures and death in heart failure a community study. J Am Coll Cardiol. 2012 Jan 17. 59(3):222-31. [Medline]. [Full Text].Ho JE, Liu C, Lyass A, Courchesne P, Pencina MJ, Vasan RS, et al. Galectin-3, a marker of cardiac fibrosis, predicts incident heart failure in the community. J Am Coll Cardiol. 2012 Oct 2. 60(14):1249-56. [Medline].Dunlay SM, Eveleth JM, Shah ND, McNallan SM, Roger VL. Medication adherence among community-dwelling patients with heart failure. Mayo Clin Proc. 2011 Apr. 86(4):273-81. [Medline]. [Full Text].Dewalt DA, Schillinger D, Ruo B, Bibbins-Domingo K, Baker DW, Holmes GM, et al. A Multisite Randomized Trial of a Single- versus Multi-Session Literacy Sensitive Self-Care Intervention for Patients with Heart Failure. Circulation. 2012 May 9. [Medline].Lindenfeld J, Albert NM, Boehmer JP, Collins SP, Ezekowitz JA, Givertz MM, et al. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010 Jun. 16(6):e1-194. [Medline].Lainscak M, Cleland JG, Lenzen MJ, Follath F, Komajda M, Swedberg K. International variations in the treatment and co-morbidity of left ventricular systolic dysfunction: data from the EuroHeart Failure Survey.Eur J Heart Fail. 2007 Mar. 9(3):292-9. [Medline].[Guideline] Peacock WF, Fonarow GC, Ander DS, Maisel A, Hollander JE, Januzzi JL Jr, et al. Society of Chest Pain Centers Recommendations for the evaluation and management of the observation stay acute heart failure patient: a report from the Society of Chest Pain Centers Acute Heart Failure Committee. Crit Pathw Cardiol. 2008 Jun. 7(2):83-6. [Medline].Steinhart B, Thorpe KE, Bayoumi AM, Moe G, Januzzi JL Jr, Mazer CD. Improving the diagnosis of acute heart failure using a validated prediction model. J Am Coll Cardiol. 2009 Oct 13. 54(16):1515-21. [Medline].Jessup M, Abraham WT, Casey DE, Feldman AM, Francis GS, Ganiats TG, et al. 2009 focused update: ACCF/AHA Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation. 2009 Apr 14. 119(14):1977-2016. [Medline].Rich MW, McSherry F, Williford WO, Yusuf S. Effect of age on mortality, hospitalizations and response to digoxin in patients with heart failure: the DIG study. J Am Coll Cardiol. 2001 Sep. 38(3):806-13. [Medline].Badve SV, Roberts MA, Hawley CM, et al. Effects of Beta-adrenergic antagonists in patients with chronic kidney disease a systematic review and meta-analysis. J Am Coll Cardiol. 2011 Sep 6. 58(11):1152-61.[Medline].Maisel AS, Krishnaswamy P, Nowak RM, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002 Jul 18. 347(3):161-7. [Medline].Januzzi JL Jr, Camargo CA, Anwaruddin S, et al. The N-terminal Pro-BNP investigation of dyspnea in the emergency department (PRIDE) study. Am J Cardiol. 2005 Apr 15. 95(8):948-54. [Medline].Wang CS, FitzGerald JM, Schulzer M, Mak E, Ayas NT. Does this dyspneic patient in the emergency department have congestive heart failure?. JAMA. 2005 Oct 19. 294(15):1944-56. [Medline].Stevenson LW, Perloff JK. The limited reliability of physical signs for estimating hemodynamics in chronic heart failure. JAMA. 1989 Feb 10. 261(6):884-8. [Medline].Pinamonti B, Di Lenarda A, Sinagra G, Camerini F. Restrictive left ventricular filling pattern in dilated cardiomyopathy assessed by Doppler echocardiography: clinical, echocardiographic and hemodynamic correlations and prognostic implications. Heart Muscle Disease Study Group. J Am Coll Cardiol. 1993 Sep. 22(3):808-15. [Medline].Temporelli PL, Scapellato F, Eleuteri E, Imparato A, Giannuzzi P. Doppler echocardiography in advanced systolic heart failure: a noninvasive alternative to Swan-Ganz catheter. Circ Heart Fail. 2010 May. 3(3):387-94. [Medline].Maisel AS, McCord J, Nowak RM, et al. Bedside B-Type natriuretic peptide in the emergency diagnosis of heart failure with reduced or preserved ejection fraction. Results from the Breathing Not Properly Multinational Study. J Am Coll Cardiol. 2003 Jun 4. 41(11):2010-7. [Medline].Januzzi JL, van Kimmenade R, Lainchbury J, et al. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: an international pooled analysis of 1256 patients: the International Collaborative of NT-proBNP Study. Eur Heart J. 2006 Feb. 27(3):330-7. [Medline].Maeda K, Tsutamoto T, Wada A, Hisanaga T, Kinoshita M. Plasma brain natriuretic peptide as a biochemical marker of high left ventricular end-diastolic pressure in patients with symptomatic left ventricular dysfunction. Am Heart J. 1998 May. 135(5 Pt 1):825-32. [Medline].Fisher C, Berry C, Blue L, Morton JJ, McMurray J. N-terminal pro B type natriuretic peptide, but not the new putative cardiac hormone relaxin, predicts prognosis in patients with chronic heart failure. Heart. 2003 Aug. 89(8):879-81. [Medline]. [Full Text].Hall C, Rouleau JL, Moye L, et al. N-terminal proatrial natriuretic factor. An independent predictor of long-term prognosis after myocardial infarction. Circulation. 1994 May. 89(5):1934-42. [Medline].Andersson B, Hall C. N-terminal proatrial natriuretic peptide and prognosis in patients with heart failure and preserved systolic function. J Card Fail. 2000 Sep. 6(3):208-13. [Medline].Chen HH, Burnett JC. Natriuretic peptides in the pathophysiology of congestive heart failure. Curr Cardiol Rep. 2000 May. 2(3):198-205. [Medline].Cheng V, Kazanagra R, Garcia A, Lenert L, Krishnaswamy P, Gardetto N, et al. A rapid bedside test for B-type peptide predicts treatment outcomes in patients admitted for decompensated heart failure: a pilot study.J Am Coll Cardiol. 2001 Feb. 37(2):386-91. [Medline].Cowie MR, Struthers AD, Wood DA, Coats AJ, Thompson SG, Poole-Wilson PA, et al. Value of natriuretic peptides in assessment of patients with possible new heart failure in primary care. Lancet. 1997 Nov 8. 350(9088):1349-53. [Medline].Dao Q, Krishnaswamy P, Kazanegra R, Harrison A, Amirnovin R, Lenert L, et al. Utility of B-type natriuretic peptide in the diagnosis of congestive heart failure in an urgent-care setting. J Am Coll Cardiol. 2001 Feb. 37(2):379-85. [Medline].Maeda K, Tsutamoto T, Wada A, Hisanaga T, Kinoshita M. Plasma brain natriuretic peptide as a biochemical marker of high left ventricular end-diastolic pressure in patients with symptomatic left ventricular dysfunction. Am Heart J. 1998 May. 135(5 Pt 1):825-32. [Medline].Maisel AS, Koon J, Hope J, et al. A rapid bedside test for brain natriuretic peptide accurately predicts cardiac function in patients referred for echocardiography. Am Heart J. 2001. 141:374-9.Masson S, Vago T, Baldi G, et al. Comparative measurement of N-terminal pro-brain natriuretic peptide and brain natriuretic peptide in ambulatory patients with heart failure. Clin Chem Lab Med. 2002 Aug. 40(8):761-3. [Medline].Song BG, Jeon ES, Kim YH, et al. Correlation between levels of N-terminal pro-B-type natriuretic peptide and degrees of heart failure. Korean J Intern Med. 2005 Mar. 20(1):26-32. [Medline].Hobbs FD, Davis RC, Roalfe AK, et al. Reliability of N-terminal pro-brain natriuretic peptide assay in diagnosis of heart failure: cohort study in representative and high risk community populations. [abstract].BMJ. 2002 Jun 22. 324(7352):1498.Redfield MM, Rodeheffer RJ, Jacobsen SJ, Mahoney DW, Bailey KR, Burnett JC Jr. Plasma brain natriuretic peptide concentration: impact of age and gender. J Am Coll Cardiol. 2002 Sep 4. 40(5):976-82. [Medline].St Peter JV, Hartley GG, Murakami MM, Apple FS. B-type natriuretic peptide (BNP) and N-terminal pro-BNP in obese patients without heart failure: relationship to body mass index and gastric bypass surgery. Clin Chem. 2006 Apr. 52(4):680-5. [Medline].Rivera M, Cortes R, Salvador A, ET AL. Obese subjects with heart failure have lower N-terminal pro-brain natriuretic peptide plasma levels irrespective of aetiology. Eur J Heart Fail. 2005 Dec. 7(7):1168-70.[Medline].Hermann-Arnhof KM, Hanusch-Enserer U, Kaestenbauer T, et al. N-terminal pro-B-type natriuretic peptide as an indicator of possible cardiovascular disease in severely obese individuals: comparison with patients in different stages of heart failure. Clin Chem. 2005 Jan. 51(1):138-43. [Medline].Seino Y, Ogawa A, Yamashita T, et al. Application of NT-proBNP and BNP measurements in cardiac care: a more discerning marker for the detection and evaluation of heart failure. Eur J Heart Fail. 2004 Mar 15. 6(3):295-300. [Medline].Colucci WS, Elkayam U, Horton DP, Abraham WT, Bourge RC, Johnson AD, et al. Intravenous nesiritide, a natriuretic peptide, in the treatment of decompensated congestive heart failure. Nesiritide Study Group. N Engl J Med. 2000 Jul 27. 343(4):246-53. [Medline].Ezekowitz JA, Hernandez AF, Starling RC, Yancy CW, Massie B, Hill JA, et al. Standardizing care for acute decompensated heart failure in a large megatrial: the approach for the Acute Studies of Clinical Effectiveness of Nesiritide in Subjects with Decompensated Heart Failure (ASCEND-HF). Am Heart J. 2009 Feb. 157(2):219-28. [Medline].Mills RM, LeJemtel TH, Horton DP, Liang C, Lang R, Silver MA, et al. Sustained hemodynamic effects of an infusion of nesiritide (human b-type natriuretic peptide) in heart failure: a randomized, double-blind, placebo-controlled clinical trial. Natrecor Study Group. J Am Coll Cardiol. 1999 Jul. 34(1):155-62. [Medline].Silver MA, Horton DP, Ghali JK, Elkayam U. Effect of nesiritide versus dobutamine on short-term outcomes in the treatment of patients with acutely decompensated heart failure. J Am Coll Cardiol. 2002 Mar 6. 39(5):798-803. [Medline].Miller WL, Hartman KA, Burritt MF, Borgeson DD, Burnett JC Jr, Jaffe AS. Biomarker responses during and after treatment with nesiritide infusion in patients with decompensated chronic heart failure. Clin Chem. 2005 Mar. 51(3):569-77. [Medline].Fitzgerald RL, Cremo R, Gardetto N, et al. Effect of nesiritide in combination with standard therapy on serum concentrations of natriuretic peptides in patients admitted for decompensated congestive heart failure. Am Heart J. 2005 Sep. 150(3):471-7. [Medline].Michels VV, Moll PP, Miller FA, et al. The frequency of familial dilated cardiomyopathy in a series of patients with idiopathic dilated cardiomyopathy. N Engl J Med. 1992 Jan 9. 326(2):77-82. [Medline].Baig MK, Goldman JH, Caforio AL, Coonar AS, Keeling PJ, McKenna WJ. Familial dilated cardiomyopathy: cardiac abnormalities are common in asymptomatic relatives and may represent early disease. J Am Coll Cardiol. 1998 Jan. 31(1):195-201. [Medline].Grunig E, Tasman JA, Kucherer H, Franz W, Kubler W, Katus HA. Frequency and phenotypes of familial dilated cardiomyopathy. J Am Coll Cardiol. 1998 Jan. 31(1):186-94. [Medline].McNally E, MacLeod H, Dellefave L. Arrhythmogenic right ventricular dysplasia/cardiomyopathy, autosomal dominant. 2005. [Medline].Cheitlin MD, Alpert JS, Armstrong WF, Aurigemma GP, Beller GA, Bierman FZ, et al. ACC/AHA Guidelines for the Clinical Application of Echocardiography. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Clinical Application of Echocardiography). Developed in collaboration with the American Society of Echocardiography. Circulation. 1997 Mar 18. 95(6):1686-744. [Medline].Patel AR, Alsheikh-Ali AA, Mukherjee J, Evangelista A, Quraini D, Ordway LJ, et al. 3D Echocardiography to Evaluate Right Atrial Pressure in Acutely Decompensated Heart Failure Correlation With Invasive Hemodynamics. JACC Cardiovasc Imaging. 2011 Sep. 4(9):938-45. [Medline].Prior D, Coller J. Echocardiography in heart failure – a guide for general practice. Aust Fam Physician. 2010 Dec. 39(12):904-9. [Medline].Kirkpatrick JN, Wiegers SE, Lang RM. Left ventricular assist devices and other devices for end-stage heart failure: utility of echocardiography. Curr Cardiol Rep. 2010 May. 12(3):257-64. [Medline].Abraham J, Abraham TP. The role of echocardiography in hemodynamic assessment in heart failure. Heart Fail Clin. 2009 Apr. 5(2):191-208. [Medline].Meersch M, Schmidt C, Zarbock A. Echophysiology: the transesophageal echo probe as a noninvasive Swan-Ganz catheter. Curr Opin Anaesthesiol. 2016 Feb. 29 (1):36-45. [Medline].Kim RJ, Wu E, Rafael A, Chen EL, Parker MA, Simonetti O, et al. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med. 2000 Nov 16. 343(20):1445-53. [Medline].Ritchie JL, Bateman TM, Bonow RO, Crawford MH, Gibbons RJ, Hall RJ, et al. Guidelines for clinical use of cardiac radionuclide imaging. Report of the American College of Cardiology/American Heart Association Task Force on Assessment of Diagnostic and Therapeutic Cardiovascular Procedures (Committee on Radionuclide Imaging), developed in collaboration with the American Society of Nuclear Cardiology. J Am Coll Cardiol. 1995 Feb. 25(2):521-47. [Medline].Taillefer R, DePuey EG, Udelson JE, Beller GA, Latour Y, Reeves F. Comparative diagnostic accuracy of Tl-201 and Tc-99m sestamibi SPECT imaging (perfusion and ECG-gated SPECT) in detecting coronary artery disease in women. J Am Coll Cardiol. 1997 Jan. 29(1):69-77. [Medline].Bonow RO, Maurer G, Lee KL, et al. Myocardial Viability and Survival in Ischemic Left Ventricular Dysfunction. N Engl J Med. 2011 Apr 4. [Medline].Binanay C, Califf RM, Hasselblad V, et al. Evaluation study of congestive heart failure and pulmonary artery catheterization effectiveness: the ESCAPE trial. JAMA. 2005 Oct 5. 294(13):1625-33. [Medline].Bitter T, Westerheide N, Prinz C, Hossain MS, Vogt J, Langer C, et al. Cheyne-Stokes respiration and obstructive sleep apnoea are independent risk factors for malignant ventricular arrhythmias requiring appropriate cardioverter-defibrillator therapies in patients with congestive heart failure. Eur Heart J. 2011 Jan. 32(1):61-74. [Medline].Groenveld HF, Januzzi JL, Damman K, et al. Anemia and mortality in heart failure patients a systematic review and meta-analysis. J Am Coll Cardiol. 2008 Sep 2. 52(10):818-27. [Medline].Ronco C, Haapio M, House AA, Anavekar N, Bellomo R. Cardiorenal syndrome. J Am Coll Cardiol. 2008 Nov 4. 52(19):1527-39. [Medline].House AA, Haapio M, Lassus J, Bellomo R, Ronco C. Therapeutic strategies for heart failure in cardiorenal syndromes. Am J Kidney Dis. 2010 Oct. 56(4):759-73. [Medline].Giamouzis G, Butler J, Starling RC, Karayannis G, Nastas J, Parisis C, et al. Impact of dopamine infusion on renal function in hospitalized heart failure patients: results of the Dopamine in Acute Decompensated Heart Failure (DAD-HF) Trial. J Card Fail. 2010 Dec. 16(12):922-30. [Medline].Pleister AP, Baliga RR, Haas GJ. Acute study of clinical effectiveness of nesiritide in decompensated heart failure: nesiritide redux. Curr Heart Fail Rep. 2011 Sep. 8(3):226-32. [Medline].Konstam MA, Gheorghiade M, Burnett JC Jr, Grinfeld L, Maggioni AP, Swedberg K, et al. Effects of oral tolvaptan in patients hospitalized for worsening heart failure: the EVEREST Outcome Trial. JAMA. 2007 Mar 28. 297(12):1319-31. [Medline].Massie BM, O’Connor CM, Metra M, Ponikowski P, Teerlink JR, Cotter G, et al. Rolofylline, an adenosine A1-receptor antagonist, in acute heart failure. N Engl J Med. 2010 Oct 7. 363(15):1419-28. [Medline].Badve SV, Roberts MA, Hawley CM, et al. Effects of Beta-adrenergic antagonists in patients with chronic kidney disease a systematic review and meta-analysis. J Am Coll Cardiol. 2011 Sep 6. 58(11):1152-61.[Medline].Roy D, Talajic M, Nattel S, et al, for the Atrial Fibrillation and Congestive Heart Failure Investigators. Rhythm control versus rate control for atrial fibrillation and heart failure. N Engl J Med. 2008 Jun 19. 358(25):2667-77. [Medline].Hsu LF, Jaïs P, Sanders P, Garrigue S, Hocini M, Sacher F, et al. Catheter ablation for atrial fibrillation in congestive heart failure. N Engl J Med. 2004 Dec 2. 351(23):2373-83. [Medline].Wilton SB, Fundytus A, Ghali WA, Veenhuyzen GD, Quinn FR, Mitchell LB, et al. Meta-analysis of the effectiveness and safety of catheter ablation of atrial fibrillation in patients with versus without left ventricular systolic dysfunction. Am J Cardiol. 2010 Nov 1. 106(9):1284-91. [Medline].MacDonald MR, Connelly DT, Hawkins NM, Steedman T, Payne J, Shaw M, et al. Radiofrequency ablation for persistent atrial fibrillation in patients with advanced heart failure and severe left ventricular systolic dysfunction: a randomised controlled trial. Heart. 2011 May. 97(9):740-7. [Medline].Chen YM, Li ZB, Zhu M, Cao YM. Effects of exercise training on left ventricular remodelling in heart failure patients: an updated meta-analysis of randomised controlled trials. Int J Clin Pract. 2012 Aug. 66(8):782-791. [Medline].Mozaffarian D, Lemaitre RN, King IB, et al. Circulating Long-Chain {omega}-3 Fatty Acids and Incidence of Congestive Heart Failure in Older Adults: The Cardiovascular Health Study: A Cohort Study. Ann Intern Med. 2011 Aug 2. 155(3):160-70. [Medline].Marchioli R, Levantesi G, Silletta MG, et al, for the GISSI-HF investigators. Effect of n-3 polyunsaturated fatty acids and rosuvastatin in patients with heart failure: results of the GISSI-HF trial. Expert Rev Cardiovasc Ther. 2009 Jul. 7(7):735-48. [Medline].Yancy CW, Jessup M, Bozkurt B, Masoudi FA, Butler J, McBride PE, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013 Jun 5. [Medline].Swedberg K, Komajda M, Bohm M, et al. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet. 2010 Sep 11. 376(9744):875-85. [Medline]. [Full Text].Borer JS, Bohm M, Ford I, et al. Effect of ivabradine on recurrent hospitalization for worsening heart failure in patients with chronic systolic heart failure: the SHIFT Study. Eur Heart J. 2012 Nov. 33(22):2813-20.[Medline]. [Full Text].US Food and Drug Administration. FDA approves new drug to treat heart failure. Available athttp://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm453845.htm. July 7, 2015; Accessed: July 8, 2015.McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014 Sep 11. 371 (11):993-1004. [Medline]. [Full Text].Solomon SD, Zile M, Pieske B, Voors A, Shah A, Kraigher-Krainer E, et al. The angiotensin receptor neprilysin inhibitor LCZ696 in heart failure with preserved ejection fraction: a phase 2 double-blind randomised controlled trial. Lancet. 2012 Oct 20. 380 (9851):1387-95. [Medline].Massie BM, Collins JF, Ammon SE, Armstrong PW, Cleland JG, Ezekowitz M, et al. Randomized trial of warfarin, aspirin, and clopidogrel in patients with chronic heart failure: the Warfarin and Antiplatelet Therapy in Chronic Heart Failure (WATCH) trial. Circulation. 2009 Mar 31. 119(12):1616-24. [Medline].Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006 Jul 20. 355(3):251-9.[Medline].Hogg K, Swedberg K, McMurray J. Heart failure with preserved left ventricular systolic function; epidemiology, clinical characteristics, and prognosis. J Am Coll Cardiol. 2004 Feb 4. 43(3):317-27.[Medline].Gheorghiade M, Abraham WT, Albert NM, et al, for the OPTIMIZE-HF Investigators and Coordinators. Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure. JAMA. 2006 Nov 8. 296(18):2217-26. [Medline].Masip J, Roque M, Sanchez B, Fernandez R, Subirana M, Exposito JA. Noninvasive ventilation in acute cardiogenic pulmonary edema: systematic review and meta-analysis. JAMA. 2005 Dec 28. 294(24):3124-30. [Medline].Peter JV, Moran JL, Phillips-Hughes J, Graham P, Bersten AD. Effect of non-invasive positive pressure ventilation (NIPPV) on mortality in patients with acute cardiogenic pulmonary oedema: a meta-analysis.Lancet. 2006 Apr 8. 367(9517):1155-63. [Medline].Winck JC, Azevedo LF, Costa-Pereira A, Antonelli M, Wyatt JC. Efficacy and safety of non-invasive ventilation in the treatment of acute cardiogenic pulmonary edema–a systematic review and meta-analysis.Crit Care. 2006. 10(2):R69. [Medline]. [Full Text].Vital FM, Saconato H, Ladeira MT, et al. Non-invasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary edema. Cochrane Database Syst Rev. 2008 Jul 16. CD005351. [Medline].Maeder MT, Kaye DM. Heart failure with normal left ventricular ejection fraction. J Am Coll Cardiol. 2009 Mar 17. 53(11):905-18. [Medline].Gray A, Goodacre S, Newby DE, Masson M, Sampson F, Nicholl J, et al. Noninvasive ventilation in acute cardiogenic pulmonary edema. N Engl J Med. 2008 Jul 10. 359(2):142-51. [Medline].The CONSENSUS Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). The CONSENSUS Trial Study Group. N Engl J Med. 1987 Jun 4. 316(23):1429-35. [Medline].The SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 1991 Aug 1. 325(5):293-302. [Medline].Zannad F, Alla F, Dousset B, Perez A, Pitt B. Limitation of excessive extracellular matrix turnover may contribute to survival benefit of spironolactone therapy in patients with congestive heart failure: insights from the randomized aldactone evaluation study (RALES). Rales Investigators. Circulation. 2000 Nov 28. 102(22):2700-6. [Medline].Busko M. Clevidipine Shows Promise for Acute HF with High BP. Medscape Medical News. Available athttp://www.medscape.com/viewarticle/820377. Accessed: February 18, 2014.Felker GM, Lee KL, Bull DA, Redfield MM, Stevenson LW, Goldsmith SR, et al. Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med. 2011 Mar 3. 364(9):797-805. [Medline].Liu PP. Cardiorenal syndrome in heart failure: a cardiologist’s perspective. Can J Cardiol. 2008 Jul. 24 suppl B:25B-9B. [Medline]. [Full Text].Kramer BK, Schweda F, Riegger GA. Diuretic treatment and diuretic resistance in heart failure. Am J Med. 1999 Jan. 106(1):90-6. [Medline].Nieminen MS, Bohm M, Cowie MR, et al for the ESC Committe for Practice Guideline (CPG). Executive summary of the guidelines on the diagnosis and treatment of acute heart failure: the Task Force on Acute Heart Failure of the European Society of Cardiology. Eur Heart J. 2005 Feb. 26(4):384-416. [Medline].Neuberg GW, Miller AB, O’Connor CM, et al. Diuretic resistance predicts mortality in patients with advanced heart failure. Am Heart J. 2002 Jul. 144(1):31-8. [Medline].Costanzo MR, Saltzberg M, O’Sullivan J, Sobotka P. Early ultrafiltration in patients with decompensated heart failure and diuretic resistance. J Am Coll Cardiol. 2005 Dec 6. 46(11):2047-51. [Medline].Young JB, Abraham WT, Stevenson LW, et al. Results of the VMAC Trial: vasodilation in the management of acute congestive heart failure. N Engl J Med. 2000. 102:a2794.Publication Committee for the VMAC Investigators (Vasodilatation in the Management of Acute CHF). Intravenous nesiritide vs nitroglycerin for treatment of decompensated congestive heart failure: a randomized controlled trial. JAMA. 2002 Mar 27. 287(12):1531-40. [Medline].Costanzo MR, Jessup M. Treatment of congestion in heart failure with diuretics and extracorporeal therapies: effects on symptoms, renal function, and prognosis. Heart Fail Rev. 2011 May 11. [Medline].Costanzo MR, Guglin ME, Saltzberg MT, Jessup ML, Bart BA, Teerlink JR, et al. Ultrafiltration versus intravenous diuretics for patients hospitalized for acute decompensated heart failure. J Am Coll Cardiol. 2007 Feb 13. 49(6):675-83. [Medline].CIBIS Investigators and Committees. A randomized trial of beta-blockade in heart failure. The Cardiac Insufficiency Bisoprolol Study (CIBIS). Circulation. 1994 Oct. 90(4):1765-73. [Medline].Chaudhry SI, Mattera JA, Curtis JP, Spertus JA, Herrin J, Lin Z, et al. Telemonitoring in patients with heart failure. N Engl J Med. 2010 Dec 9. 363(24):2301-9. [Medline].Koehler F, Winkler S, Schieber M, et al. Impact of Remote Telemedical Management on Mortality and Hospitalizations in Ambulatory Patients With Chronic Heart Failure: The Telemedical Interventional Monitoring in Heart Failure Study. Circulation. 2011 May 3. 123(17):1873-1880. [Medline].US Food and Drug Administration. FDA approves first implantable wireless device with remote monitoring to measure pulmonary artery pressure in certain heart failure patients (news release). Available athttp://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm399024.htm. Accessed: June 2, 2014.O’Riordan M. FDA approves first implantable device for remotely monitoring HF patients. Heartwire. May 28, 2014. [Full Text].Abraham WT, Adamson PB, Bourge RC, Aaron MF, Costanzo MR, Stevenson LW, et al. Wireless pulmonary artery haemodynamic monitoring in chronic heart failure: a randomised controlled trial. Lancet. 2011 Feb 19. 377(9766):658-66. [Medline].Eisen HJ, Kobashigawa J, Keogh A, Bourge R, Renlund D, Mentzer R, et al. Three-year results of a randomized, double-blind, controlled trial of mycophenolate mofetil versus azathioprine in cardiac transplant recipients. J Heart Lung Transplant. 2005 May. 24(5):517-25. [Medline].Yancy CW, Lopatin M, Stevenson LW, De Marco T, Fonarow GC. Clinical presentation, management, and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: a report from the Acute Decompensated Heart Failure National Registry (ADHERE) Database. J Am Coll Cardiol. 2006 Jan 3. 47(1):76-84. [Medline].Dickstein K, Vardas PE, Auricchio A, et al al for the Task Force on Acute Heart Failure of the European Society of Cardiology. 2010 Focused Update of ESC Guidelines on device therapy in heart failure: an update of the 2008 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure and the 2007 ESC guidelines for cardiac and resynchronization therapy. Developed with the special contribution of the Heart Failure Association and the European Heart Rhythm Association. Eur Heart J. 2010 Nov. 31(21):2677-87. [Medline].Tracy CM, Epstein AE, Darbar D, Dimarco JP, Dunbar SB, Estes NA 3rd, et al. 2012 ACCF/AHA/HRS Focused Update of the 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2012 Sep 10. [Medline].Miller R. AHA issues mechanical circulatory-support guidance for referring docs. Medscape Medical News. November 1, 2012. [Full Text].Peura JL, Colvin-Adams M, Francis GS, et al, on behalf of the American Heart Association Heart Failure and Transplantation Committee of the Council on Clinical Cardiology, Council on Cardiopulmonary, et al. Recommendations for the Use of Mechanical Circulatory Support: Device Strategies and Patient Selection: A Scientific Statement From the American Heart Association. Circulation. 2012 Oct 29. [Medline].FDA news release. FDA approves expanded indication for certain pacemakers and defibrillators used to treat heart failure. US Food and Drug Administration. Available athttp://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm392861.htm. Accessed: April 14, 2014.Stiles S. FDA Approves Medtronic CRT Devices for Mild HF With AV Block. Medscape [serial online]. Available at http://www.medscape.com/viewarticle/823485. Accessed: April 14, 2014.Levy WC, Lee KL, Hellkamp AS, Poole JE, Mozaffarian D, Linker DT, et al. Maximizing survival benefit with primary prevention implantable cardioverter-defibrillator therapy in a heart failure population. Circulation. 2009 Sep 8. 120(10):835-42. [Medline].Rosanio S, Schwarz ER, Ahmad M, Jammula P, Vitarelli A, Uretsky BF, et al. Benefits, unresolved questions, and technical issues of cardiac resynchronization therapy for heart failure. Am J Cardiol. 2005 Sep 1. 96(5):710-7. [Medline].Tang AS, Wells GA, Talajic M, Arnold MO, Sheldon R, Connolly S, et al. Cardiac-resynchronization therapy for mild-to-moderate heart failure. N Engl J Med. 2010 Dec 16. 363(25):2385-95. [Medline].Giraldi F, Cattadori G, Roberto M, et al. Long-term effectiveness of cardiac resynchronization therapy in heart failure patients with unfavorable cardiac veins anatomy comparison of surgical versus hemodynamic procedure. J Am Coll Cardiol. 2011 Jul 26. 58(5):483-90. [Medline].Abraham WT, Fisher WG, Smith AL, Delurgio DB, Leon AR, Loh E, et al. Cardiac resynchronization in chronic heart failure. N Engl J Med. 2002 Jun 13. 346(24):1845-53. [Medline].Moss AJ, Hall WJ, Cannom DS, Klein H, Brown MW, Daubert JP, et al. Cardiac-resynchronization therapy for the prevention of heart-failure events. N Engl J Med. 2009 Oct 1. 361(14):1329-38. [Medline].Arshad A, Moss AJ, Foster E, Padeletti L, Barsheshet A, Goldenberg I, et al. Cardiac resynchronization therapy is more effective in women than in men: the MADIT-CRT (Multicenter Automatic Defibrillator Implantation Trial with Cardiac Resynchronization Therapy) trial. J Am Coll Cardiol. 2011 Feb 15. 57(7):813-20. [Medline].Ruwald MH, Ruwald AC, Jons C, Alexis J, McNitt S, Zareba W, et al. Effect of Metoprolol Versus Carvedilol on Outcomes in MADIT-CRT (Multicenter Automatic Defibrillator Implantation Trial With Cardiac Resynchronization Therapy). J Am Coll Cardiol. 2013 Apr 9. 61(14):1518-26. [Medline].Cleland JG, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005 Apr 14. 352(15):1539-49.[Medline].Bristow MR, Saxon LA, Boehmer J, Krueger S, Kass DA, De Marco T, et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med. 2004 May 20. 350(21):2140-50. [Medline].Curtis AB, Worley SJ, Adamson PB, Chung ES, Niazi I, Sherfesee L, et al. Biventricular pacing for atrioventricular block and systolic dysfunction. N Engl J Med. 2013 Apr 25. 368(17):1585-93. [Medline].Emery G. Biventricular pacing better for heart failure patients. Medscape Medical News. April 24, 2013. [Full Text].Caracciolo EA, Davis KB, Sopko G, Kaiser GC, Corley SD, Schaff H, et al. Comparison of surgical and medical group survival in patients with left main equivalent coronary artery disease. Long-term CASS experience. Circulation. 1995 May 1. 91(9):2335-44. [Medline].Eleven-year survival in the Veterans Administration randomized trial of coronary bypass surgery for stable angina. The Veterans Administration Coronary Artery Bypass Surgery Cooperative Study Group. N Engl J Med. 1984 Nov 22. 311(21):1333-9. [Medline].Robinson TN, Morrell TD, Pomerantz BJ, Heimbach JK, Cairns CB, Harken AH. Therapeutically accessible clinical cardiac states. J Am Coll Surg. 2000 Oct. 191(4):452-63. [Medline].Senior R, Lahiri A, Kaul S. Effect of revascularization on left ventricular remodeling in patients with heart failure from severe chronic ischemic left ventricular dysfunction. Am J Cardiol. 2001 Sep 15. 88(6):624-9.[Medline].Velazquez EJ, Lee KL, Deja MA, Jain A, Sopko G, Marchenko A, et al. Coronary-Artery Bypass Surgery in Patients with Left Ventricular Dysfunction. N Engl J Med. 2011 Apr 4. [Medline]. [Full Text].Elefteriades JA, Morales DL, Gradel C, Tollis G Jr, Levi E, Zaret BL. Results of coronary artery bypass grafting by a single surgeon in patients with left ventricular ejection fractions < or = 30%. Am J Cardiol. 1997 Jun 15. 79(12):1573-8. [Medline].Kron IL, Flanagan TL, Blackbourne LH, Schroeder RA, Nolan SP. Coronary revascularization rather than cardiac transplantation for chronic ischemic cardiomyopathy. Ann Surg. 1989 Sep. 210(3):348-52; discussion 352-4. [Medline]. [Full Text].Doenst T, Velazquez EJ, Beyersdorf F, Michler R, Menicanti L, Di Donato M, et al. To STICH or not to STICH: we know the answer, but do we understand the question?. J Thorac Cardiovasc Surg. 2005 Feb. 129(2):246-9. [Medline].Joyce D, Loebe M, Noon GP, McRee S, Southard R, Thompson L, et al. Revascularization and ventricular restoration in patients with ischemic heart failure: the STICH trial. Curr Opin Cardiol. 2003 Nov. 18(6):454-7.[Medline].Sharoni E, Song HK, Peterson RJ, Guyton RA, Puskas JD. Off pump coronary artery bypass surgery for significant left ventricular dysfunction: safety, feasibility, and trends in methodology over time–an early experience. Heart. 2006 Apr. 92(4):499-502. [Medline]. [Full Text].Calafiore AM, Di Giammarco G, Teodori G, et al. Late results of first myocardial revascularization in multiple vessel disease: single versus bilateral internal mammary artery with or without saphenous vein grafts. Eur J Cardiothorac Surg. 2004 Sep. 26(3):542-8. [Medline].Nishimura RA, Grantham JA, Connolly HM, Schaff HV, Higano ST, Holmes DR Jr. Low-output, low-gradient aortic stenosis in patients with depressed left ventricular systolic function: the clinical utility of the dobutamine challenge in the catheterization laboratory. Circulation. 2002 Aug 13. 106(7):809-13. [Medline].Carabello BA. Clinical practice. Aortic stenosis. N Engl J Med. 2002 Feb 28. 346(9):677-82. [Medline].Lindblom D, Lindblom U, Qvist J, Lundström H. Long-term relative survival rates after heart valve replacement. J Am Coll Cardiol. 1990 Mar 1. 15(3):566-73. [Medline].Connolly HM, Oh JK, Schaff HV, Roger VL, Osborn SL, Hodge DO, et al. Severe aortic stenosis with low transvalvular gradient and severe left ventricular dysfunction:result of aortic valve replacement in 52 patients. Circulation. 2000 Apr 25. 101(16):1940-6. [Medline].deFilippi CR, Willett DL, Brickner ME, Appleton CP, Yancy CW, Eichhorn EJ, et al. Usefulness of dobutamine echocardiography in distinguishing severe from nonsevere valvular aortic stenosis in patients with depressed left ventricular function and low transvalvular gradients. Am J Cardiol. 1995 Jan 15. 75(2):191-4. [Medline].Vaquette B, Corbineau H, Laurent M, Lelong B, Langanay T, de Place C, et al. Valve replacement in patients with critical aortic stenosis and depressed left ventricular function: predictors of operative risk, left ventricular function recovery, and long term outcome. Heart. 2005 Oct. 91(10):1324-9. [Medline]. [Full Text].Dujardin KS, Enriquez-Sarano M, Schaff HV, Bailey KR, Seward JB, Tajik AJ. Mortality and morbidity of aortic regurgitation in clinical practice. A long-term follow-up study. Circulation. 1999 Apr 13. 99(14):1851-7.[Medline].Chaliki HP, Mohty D, Avierinos JF, Scott CG, Schaff HV, Tajik AJ, et al. Outcomes after aortic valve replacement in patients with severe aortic regurgitation and markedly reduced left ventricular function.Circulation. 2002 Nov 19. 106(21):2687-93. [Medline].Enriquez-Sarano M, Tajik AJ. Clinical practice. Aortic regurgitation. N Engl J Med. 2004 Oct 7. 351(15):1539-46. [Medline].Lancellotti P, Gérard PL, Piérard LA. Long-term outcome of patients with heart failure and dynamic functional mitral regurgitation. Eur Heart J. 2005 Aug. 26(15):1528-32. [Medline].Patel JB, Borgeson DD, Barnes ME, Rihal CS, Daly RC, Redfield MM. Mitral regurgitation in patients with advanced systolic heart failure. J Card Fail. 2004 Aug. 10(4):285-91. [Medline].Bolling SF, Pagani FD, Deeb GM, Bach DS. Intermediate-term outcome of mitral reconstruction in cardiomyopathy. J Thorac Cardiovasc Surg. 1998 Feb. 115(2):381-6; discussion 387-8. [Medline].Akasaka T, Yoshida K, Hozumi T, Takagi T, Kaji S, Kawamoto T, et al. Restricted coronary flow reserve in patients with mitral regurgitation improves after mitral reconstructive surgery. J Am Coll Cardiol. 1998 Dec. 32(7):1923-30. [Medline].Wu AH, Aaronson KD, Bolling SF, Pagani FD, Welch K, Koelling TM. Impact of mitral valve annuloplasty on mortality risk in patients with mitral regurgitation and left ventricular systolic dysfunction. J Am Coll Cardiol. 2005 Feb 1. 45(3):381-7. [Medline].McGee EC, Gillinov AM, Blackstone EH, Rajeswaran J, Cohen G, Najam F, et al. Recurrent mitral regurgitation after annuloplasty for functional ischemic mitral regurgitation. J Thorac Cardiovasc Surg. 2004 Dec. 128(6):916-24. [Medline].Srichai MB, Grimm RA, Stillman AE, Gillinov AM, Rodriguez LL, Lieber ML, et al. Ischemic mitral regurgitation: impact of the left ventricle and mitral valve in patients with left ventricular systolic dysfunction.Ann Thorac Surg. 2005 Jul. 80(1):170-8. [Medline].Morishita A, Shimakura T, Nonoyama M, Takasaki T. Mitral valve replacement in ischemic mitral regurgitation. Preservation of both anterior and posterior mitral leaflets. J Cardiovasc Surg (Torino). 2002 Apr. 43(2):147-52. [Medline].Yun KL, Sintek CF, Miller DC, Pfeffer TA, Kochamba GS, Khonsari S, et al. Randomized trial comparing partial versus complete chordal-sparing mitral valve replacement: effects on left ventricular volume and function. J Thorac Cardiovasc Surg. 2002 Apr. 123(4):707-14. [Medline].Gillinov AM, Wierup PN, Blackstone EH, Bishay ES, Cosgrove DM, White J, et al. Is repair preferable to replacement for ischemic mitral regurgitation?. J Thorac Cardiovasc Surg. 2001 Dec. 122(6):1125-41.[Medline].Miller DC. Ischemic mitral regurgitation redux–to repair or to replace?. J Thorac Cardiovasc Surg. 2001 Dec. 122(6):1059-62. [Medline].Feldman T, Kar S, Rinaldi M, Fail P, Hermiller J, Smalling R, et al. Percutaneous mitral repair with the MitraClip system: safety and midterm durability in the initial EVEREST (Endovascular Valve Edge-to-Edge REpair Study) cohort. J Am Coll Cardiol. 2009 Aug 18. 54(8):686-94. [Medline].Buckberg GD. Ventricular restoration–a surgical approach to reverse ventricular remodeling. Heart Fail Rev. 2004 Oct. 9(4):233-9; discussion 347-51. [Medline].Yamaguchi A, Ino T, Adachi H, Murata S, Kamio H, Okada M, et al. Left ventricular volume predicts postoperative course in patients with ischemic cardiomyopathy. Ann Thorac Surg. 1998 Feb. 65(2):434-8.[Medline].Mickleborough LL, Carson S, Ivanov J. Repair of dyskinetic or akinetic left ventricular aneurysm: results obtained with a modified linear closure. J Thorac Cardiovasc Surg. 2001 Apr. 121(4):675-82. [Medline].Ott DA, Parravacini R, Cooley DA, DePuey EG, Reul GJ, Duncan JM, et al. Improved cardiac function following left ventricular aneurysm resection: pre- and postoperative performance studies in 150 patients.Tex Heart Inst J. 1982 Sep. 9(3):267-73. [Medline]. [Full Text].Athanasuleas CL, Buckberg GD, Stanley AW, Siler W, Dor V, Di Donato M, et al. Surgical ventricular restoration in the treatment of congestive heart failure due to post-infarction ventricular dilation. J Am Coll Cardiol. 2004 Oct 6. 44(7):1439-45. [Medline].Jones RH, Velazquez EJ, Michler RE, et al. Coronary bypass surgery with or without surgical ventricular reconstruction. N Engl J Med. 2009 Apr 23. 360(17):1705-17. [Medline]. [Full Text].Timms D. A review of clinical ventricular assist devices. Med Eng Phys. 2011 Jun 10. [Medline].Pamboukian SV, Tallaj JA, Brown RN, Holman WL, Blood M, George JF, et al. Improvement in 2-year survival for ventricular assist device patients after implementation of an intensive surveillance protocol. J Heart Lung Transplant. 2011 Aug. 30(8):879-87. [Medline].Lietz K, Long JW, Kfoury AG, Slaughter MS, Silver MA, Milano CA, et al. Outcomes of left ventricular assist device implantation as destination therapy in the post-REMATCH era: implications for patient selection.Circulation. 2007 Jul 31. 116(5):497-505. [Medline].Daneshmand MA, Rajagopal K, Lima B, Khorram N, Blue LJ, Lodge AJ, et al. Left ventricular assist device destination therapy versus extended criteria cardiac transplant. Ann Thorac Surg. 2010 Apr. 89(4):1205-9; discussion 1210. [Medline].Rose EA, Gelijns AC, Moskowitz AJ, Heitjan DF, Stevenson LW, Dembitsky W, et al. Long-term use of a left ventricular assist device for end-stage heart failure. N Engl J Med. 2001 Nov 15. 345(20):1435-43.[Medline].Park SJ, Tector A, Piccioni W, Raines E, Gelijns A, Moskowitz A, et al. Left ventricular assist devices as destination therapy: a new look at survival. J Thorac Cardiovasc Surg. 2005 Jan. 129(1):9-17. [Medline].Starling RC, Naka Y, Boyle AJ, Gonzalez-Stawinski G, John R, Jorde U, et al. Results of the post-U.S. Food and Drug Administration-approval study with a continuous flow left ventricular assist device as a bridge to heart transplantation: a prospective study using the INTERMACS (Interagency Registry for Mechanically Assisted Circulatory Support). J Am Coll Cardiol. 2011 May 10. 57(19):1890-8. [Medline].Ventura PA, Alharethi R, Budge D, Reid BB, Horne BD, Mason NO, et al. Differential impact on post-transplant outcomes between pulsatile- and continuous-flow left ventricular assist devices. Clin Transplant. 2011 Jul. 25(4):E390-5. [Medline].Slaughter MS, Pagani FD, et al, for the HeartMate II Clinical Investigators. Clinical management of continuous-flow left ventricular assist devices in advanced heart failure. J Heart Lung Transplant. 2010 Apr. 29(4 suppl):S1-39. [Medline].Kirklin JK, Naftel DC, Kormos RL, et al. Third INTERMACS Annual Report: the evolution of destination therapy in the United States. J Heart Lung Transplant. 2011 Feb. 30(2):115-23. [Medline].Taylor DO, Edwards LB, Boucek MM, Trulock EP, Deng MC, Keck BM, et al. Registry of the International Society for Heart and Lung Transplantation: twenty-second official adult heart transplant report–2005. J Heart Lung Transplant. 2005 Aug. 24(8):945-55. [Medline].Boucek MM, Edwards LB, Keck BM, Trulock EP, Taylor DO, Hertz MI. Registry of the International Society for Heart and Lung Transplantation: eighth official pediatric report–2005. J Heart Lung Transplant. 2005 Aug. 24(8):968-82. [Medline].Stevenson LW, Kormos RL, Bourge RC, Gelijns A, Griffith BP, Hershberger RE, et al. Mechanical cardiac support 2000: current applications and future trial design. June 15-16, 2000 Bethesda, Maryland. J Am Coll Cardiol. 2001 Jan. 37(1):340-70. [Medline].Gray NA Jr, Selzman CH. Current status of the total artificial heart. Am Heart J. 2006 Jul. 152(1):4-10.[Medline].Cooley DA, Liotta D, Hallman GL, Bloodwell RD, Leachman RD, Milam JD. Orthotopic cardiac prosthesis for two-staged cardiac replacement. Am J Cardiol. 1969 Nov. 24(5):723-30. [Medline].Platis A, Larson DF. CardioWest temporary total artificial heart. Perfusion. 2009 Sep. 24(5):341-6. [Medline].Roussel JC, Senage T, Baron O, et al. CardioWest (Jarvik) total artificial heart: a single-center experience with 42 patients. Ann Thorac Surg. 2009 Jan. 87(1):124-9; discussion 130. [Medline].Anderson E, Jaroszewski D, Pierce C, DeValeria P, Arabia F. Parallel application of extracorporeal membrane oxygenation and the CardioWest total artificial heart as a bridge to transplant. Ann Thorac Surg. 2009 Nov. 88(5):1676-8. [Medline].Morris RJ. Total artificial heart–concepts and clinical use. Semin Thorac Cardiovasc Surg. 2008 Fall. 20(3):247-54. [Medline].Meyer A, Slaughter M. The total artificial heart. Panminerva Med. 2011 Sep. 53(3):141-54. [Medline].Anand IS, Carson P, Galle E, Song R, Boehmer J, Ghali JK, et al. Cardiac resynchronization therapy reduces the risk of hospitalizations in patients with advanced heart failure: results from the Comparison of Medical Therapy, Pacing and Defibrillation in Heart Failure (COMPANION) trial. Circulation. 2009 Feb 24. 119(7):969-77. [Medline].[Guideline] Bangalore S, Kumar S, Messerli FH. When conventional heart failure therapy is not enough: angiotensin receptor blocker, direct renin inhibitor, or aldosterone antagonist?. Congest Heart Fail. 2012 Dec 12. [Medline].Libby, Bonow, Mann, Zipes. Braunwald’s Heart Disease a Textbook of Cardiovascular Medicine. 8th edition. 2008. 509-727.Cleland JG, Teerlink JR, Senior R, Nifontov EM, Mc Murray JJ, Lang CC, et al. The effects of the cardiac myosin activator, omecamtiv mecarbil, on cardiac function in systolic heart failure: a double-blind, placebo-controlled, crossover, dose-ranging phase 2 trial. Lancet. 2011 Aug 20. 378(9792):676-83. [Medline].DeBakey ME. Development of mechanical heart devices. Ann Thorac Surg. 2005 Jun. 79(6):S2228-31.[Medline].[Guideline] DiDomenico RJ, Park HY, Southworth MR, Eyrich HM, Lewis RK, Finley JM, et al. Guidelines for acute decompensated heart failure treatment. Ann Pharmacother. 2004 Apr. 38(4):649-60. [Medline].Eklind-Cervenka M, Benson L, Dahlstrom U, Edner M, Rosenqvist M, Lund LH. Association of candesartan vs losartan with all-cause mortality in patients with heart failure. JAMA. 2011 Jan 12. 305(2):175-82.[Medline].[Guideline] Feldman D, Pamboukian SV, Teuteberg JJ, et al. The 2013 International Society for Heart and Lung Transplantation Guidelines for Mechanical Circulatory Support: Executive Summary. J Heart Lung Transplant. 2013. 32:157-187.Freeman JV, Yang J, Sung SH, Hlatky MA, Go AS. Effectiveness and safety of digoxin among contemporary adults with incident systolic heart failure. Circ Cardiovasc Qual Outcomes. 2013 Sep 1. 6(5):525-33.[Medline].Fumoto H, Horvath DJ, Rao S, Massiello AL, Horai T, Takaseya T, et al. In vivo acute performance of the Cleveland Clinic self-regulating, continuous-flow total artificial heart. J Heart Lung Transplant. 2010 Jan. 29(1):21-6. [Medline]. [Full Text].Jarcho JA. Biventricular pacing. N Engl J Med. 2006 Jul 20. 355(3):288-94. [Medline].Jennings DL, Chambers RM, Schillig JM. The pharmacotherapy of the HeartMate II, a continuous flow left ventricular assist device, in patients with advanced heart failure: integration of disease, device, and drug.Ann Pharmacother. 2010 Oct. 44(10):1647-50. [Medline].Opie LH. Digitalis, yesterday and today, but not forever. Circ Cardiovasc Qual Outcomes. 2013 Sep 1. 6(5):511-3. [Medline].Plank B, Kutyifa V, Moss AJ, Huang DT, Ruwald AC, McNitt S, et al. Smoking is Associated with an Increased Risk of First and Recurrent Ventricular Tachyarrhythmias in Mild Heart Failure Patients with Ischemic and Non-Ischemic Cardiomyopathy – A MADIT-CRT Sub-Study. Heart Rhythm. 2014 Feb 6.[Medline].Stiles S. Doubling down on RAAS blockade in HF? Aldosterone antagonists, not ARBs, says meta-analysis.Medscape. Dec 26 2012. [Full Text].Stiles S. Smoking Can Up Risk of Delivered ICD Therapy in Mild HF. Medscape Medical News. Available athttp://www.medscape.com/viewarticle/820637. Accessed: March 2, 2014.Stiles S. A Walk Through Long-Term Mechanical Circulatory Support: New ISHLT Guidelines. Available athttp://www.medscape.com/viewarticle/777744. Accessed: January 23, 2013.Stiles S. Friend or Foe? Digoxin for Systolic HF Ups Mortality in Cohort Study. Medscape Medical News. Available at http://www.medscape.com/viewarticle/811298. Accessed: September 24, 2013.Topilsky Y, Oh JK, Atchison FW, Shah DK, Bichara VM, Schirger JA, et al. Echocardiographic findings in stable outpatients with properly functioning HeartMate II left ventricular assist devices. J Am Soc Echocardiogr. 2011 Feb. 24(2):157-69. [Medline].Yancy CW, Jessup M, Bozkurt B, Masoudi FA, Butler J, McBride PE, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013 Jun 5. [Medline].Haddad F, Elmi-Sarabi M, Fadel E, Mercier O, Denault AY. Pearls and pitfalls in managing right heart failure in cardiac surgery. Curr Opin Anaesthesiol. 2016 Feb. 29 (1):68-79. [Medline].Bois JP, Chareonthaitawee P. Radionuclide imaging in congestive heart failure: assessment of viability, sarcoidosis, and amyloidosis. Cardiol Clin. 2016 Feb. 34 (1):119-32. [Medline].








